Insulin therapy is one of the important means to achieve good blood sugar control. Insulin injection device and injection technique are important aspects of insulin treatment. Surveys show that irregular injections are common, and the current situation of injections for diabetic patients in my country is even more dire.
Usually, diabetic patients have certain psychological barriers to drug injection, such as anxiety and fear. Therefore, before injecting insulin, appropriate psychological counseling should be provided to help patients overcome psychological barriers, or hidden needle equipment should be used for injection.
1Injection sites and precautions for various types of insulin
According to the characteristics of pharmacokinetics, clinical insulin preparations can be divided into ultra-short-acting (rapid-acting) insulin analogs, short-acting (regular) insulin, intermediate-acting insulin, and long-acting insulin preparations (including long-acting insulin and long-acting insulin analogues). products) and premixed insulin preparations (including premixed insulin and premixed insulin analogs).
The rate of absorption of ultra-short-acting (fast-acting) insulin analogs is not affected by the injection site and can be injected subcutaneously at any injection site. Short-acting insulin is absorbed faster under the skin of the abdomen, so the abdomen is the preferred site for injection. Intramuscular injections of intermediate-acting and long-acting insulin must be strictly avoided due to the risk of hypoglycemia. Insulin is absorbed more slowly in the thighs and buttocks, so the preferred injection site for basal insulin is the thighs and buttocks.
To reduce the risk of nocturnal hypoglycemia, intermediate-acting insulin should be administered at bedtime as much as possible and avoid administration at dinner. Hypoglycemia warnings must be given to patients who exercise after receiving long-acting subcutaneous injections of insulin. When injecting regular premixed insulin preparations before breakfast, the preferred injection site is abdominal subcutaneous to speed up the absorption of regular (short-acting) insulin and facilitate control of blood sugar fluctuations after breakfast. When injecting premixed insulin preparations before dinner, the preferred injection site is the buttocks or thigh subcutaneously to delay the absorption of intermediate-acting insulin and reduce the occurrence of nighttime hypoglycemia.
Glucagon-like peptide 1 (GLP-1) receptor agonists can be injected subcutaneously at any conventional injection site. The rotation of the injection site and the selection of needle length should follow existing recommendations for insulin injection.
2 Precautions when using insulin pens
To prevent the spread of infectious diseases, insulin pens, refills and medicine bottles cannot be shared. One stroke per person. In order to prevent air or other contaminants from entering the pen core and leaking of the medicine solution, affecting the dose accuracy, the needle of the insulin pen should be discarded after use and must not be left on the insulin pen. Wait at least 10 seconds before withdrawing the needle from the injected drug to ensure that all the drug is injected into the body and to prevent leakage of the drug solution. For larger doses, it may be necessary to exceed 10 s. The standard injection of insulin is as follows:
Standard 9 steps for insulin injection (insulin pen)
3 Precautions when using special insulin syringes
Insulin syringes are still frequently used in China. It must be noted that appropriate syringes (such as U-40, U-100) should be used for different concentrations of insulin. Before withdrawing insulin, use a syringe to inhale a volume of air equivalent to the insulin dose, and then inject the air into the insulin bottle to make the insulin easier to withdraw. If there are air bubbles in the syringe, gently tap the syringe barrel to allow the air bubbles to accumulate on the liquid surface at the upper part of the syringe, and then push the inner plug to expel the air bubbles. Unlike an insulin pen, the inner plug of the syringe can be pulled out by pushing it in place without leaving it under the skin for 10 seconds. Syringes are for single use only.
4 Precautions for insulin pump application
The insulin pump is an insulin input device controlled by artificial intelligence. It simulates the physiological secretion of insulin in the human body through continuous subcutaneous insulin infusion (CSII). Anyone who uses an insulin pump should learn how to rotate injection sites (Figure 2). This rotation includes rotation between different injection sites and rotation within the same injection site (Figure 3).
Recommended injection sites
Injection site rotation options: Numbers indicate different areas available for rotation
If patients experience any unexplained blood sugar changes (frequent hypoglycemia or hyperglycemia), they should check the injection site for fat hyperplasia, nodules, scars, inflammation, or other skin and subcutaneous conditions that affect insulin flow and absorption. Patients should frequently check their infusion sites, and healthcare professionals should examine patients at least once a year to confirm whether there is subcutaneous fat hyperplasia.
Patients should consider using the shortest needles and catheters available to reduce the risk of intramuscular injections. Young children and thinner individuals may need injections into the skin. Patients should consider using the smallest diameter needles and catheters to reduce pain and needle failure. If complications occur at the infusion site with a vertical needle line, the use of an angled needle should be considered.
5 Selection and precautions for insulin pen needles
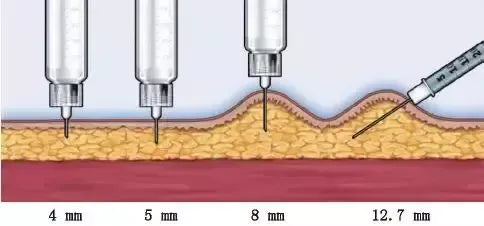
The goal of diabetes drug injection is to reliably deliver the drug into the subcutaneous tissue to ensure no leakage and no discomfort. Choosing the right needle length is key. Regardless of whether the skin is pinched or not, the 4 mm needle should be inserted vertically. When injecting, you should avoid pressing the skin to create depressions to prevent the needle from penetrating too deep into the muscle tissue. If you use a needle of 6 mm and above to inject in the upper arm, you must pinch the skin, which requires the assistance of another person to complete the injection. Patients who are unable to hold an insulin pen with a 4 mm needle due to hand tremors or other impairments may need to use a longer needle. When injecting into the limbs or the abdomen with less fat, to prevent intramuscular injection, pinch the skin for injection even when using 4 mm and 5 mm needles. When using a 6 mm needle, skin pinch or 45° injection can be used. Needle insertion angles when using needles of various lengths for injection
Young children and very thin adults should use a 4 mm needle and insert the needle vertically by pinching the skin. Other people use a 4 mm needle for injection without pinching the skin. If only an 8 mm needle is available to the patient (such as a patient currently using a syringe), the skin should be pinched and injected at 45°. For obese patients, 4 mm needles are safe and effective, and 5 mm needles are also acceptable.